If you or your child have health coverage through Medicaid or the Children’s Health Insurance Program (CHIP), learn how to update your information so you don't lose coverage.
Among the Best
Our hospital in Delaware is ranked by U.S. News & World Report in five specialties and our hospital in Florida is ranked in two.


In Our Leader’s Own Words
Our president and CEO, Dr. Larry Moss, is a thought leader in the transformation of children’s health. See what he has to say in his published white papers, blog articles, news articles and videos.
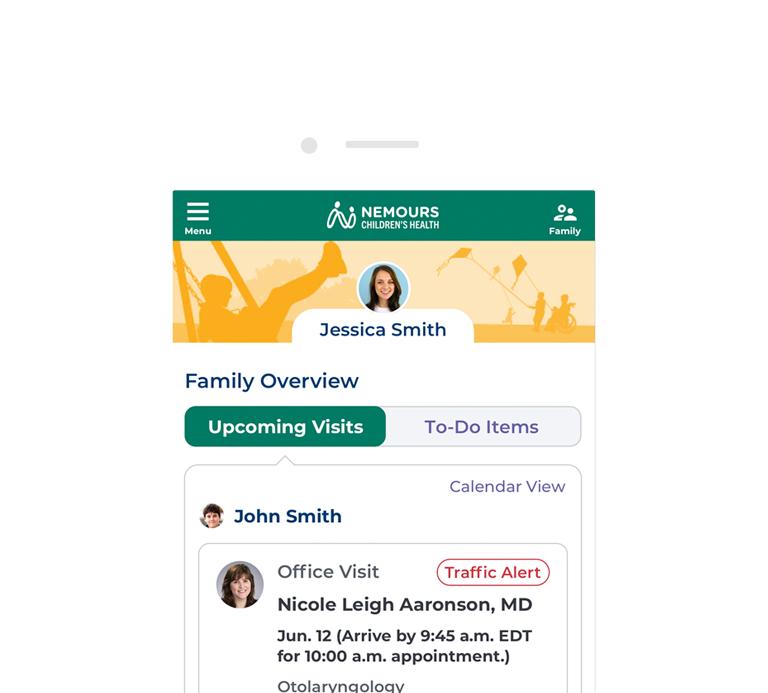
The Nemours App
You can schedule appointments, view test results, refill prescriptions, message the doctor and more.
In the Loop
Life-Changing Research
Nemours Children's is leading important pediatric research and clinical trials. We’re preventing and reversing the course of childhood diseases, improving health care delivery and keeping children safe and healthy for generations to come. We partner with renowned medical schools and organizations to find answers to the most pressing questions in kids’ health. Our discoveries help children in your community and all over the world.

Careers — Positions Available Immediately
There’s never been a better time to join our team — we’re hiring nurses, physicians, medical assistants and many more.
Donations and Volunteering
Nemours Children's has set out to change the definition of children’s health. We believe good health goes beyond great medicine. Good health involves education and access to food and housing. It includes strong families. It addresses mental wellness, health equity and justice for all. And so much more. Join us.