Sleep Medicine
Helping Kids Get a Better Night’s Rest
Nemours Children's sleep medicine experts help kids grow, develop and live healthy. We work to improve sleep in children of all ages, from babies to teens.
Our programs are led by renowned specialists in pediatric pulmonology and neurology who are also trained in sleep medicine. We use the latest tools to understand why children have trouble sleeping. With the right diagnosis, we can help kids get back to sleep.
We see a lot of children with sleep disorders and know what to look for. We consider breathing problems, developmental issues, physical problems, sleep habits and more. We also help kids with complex health conditions that can cause or be related to poor sleep.
We work as a team to help your child sleep better, so they can learn, focus and be their very best.
Conditions & Treatments
Many types of sleep disorders in children, medical conditions and complex medical needs can contribute to sleep problems. We see a full spectrum of conditions — far too many to list here. Don't see a condition listed? Call us.
Related Specialties
“We have received so much support here at Nemours. Dr. Chidekel was with us every step of the way during her sleep studies.”
What’s so important about sleep? Find out everything you need to know from the experts at Nemours KidsHealth.org.
Toddler sleep tips. Learn how to build good sleeping habits for a lifetime of good health.
We’re Experts at Getting Kids Back to Sleep
Nemours board-certified sleep medicine specialists are experts in sleep disorders. We know how sleep affects a child’s body, behavior, learning and more.
11
8 hours
12+
Delaware Valley/Philadelphia Highlights
Our program is accredited. The American Academy of Sleep Medicine recognizes our pediatric sleep program for the highest in quality and safety.
We’re regional pioneers in coordinated sleep care. Ours was the first hospital in the Delaware Valley to offer same-day pulmonology and otolaryngology (ear, nose and throat, or ENT) sleep services for kids with complex breathing problems. We bring the right care to families, when and where you need it.
We offer specialized sleep programs. Our teams work together to help kids with special health needs sleep better. We have expertise in neuromuscular disorders, epilepsy, autism spectrum disorders and craniofacial disorders.
We’re Experts at Getting Kids Back to Sleep
Nemours board-certified sleep medicine specialists are experts in sleep disorders. We know how sleep affects a child’s body, behavior, learning and more.
11
8 hours
12+
Florida Highlights
Our program is accredited. The American Academy of Sleep Medicine recognizes the sleep center at Wolfson Children’s Hospital, which is led by our team, for the highest in quality and safety.
We have state-of-the-art sleep centers just for kids. We provide sleep studies in private, kid-friendly rooms. While your child sleeps, we can record a variety of body functions to help us understand what’s going on. You can sleep in the same room with your child, next to their bed.
We offer specialized sleep programs. Our teams work together to help kids with special health needs sleep better. We have expertise in neuromuscular disorders, epilepsy, autism spectrum disorders and craniofacial disorders.
We’re Experts at Getting Kids Back to Sleep
Nemours board-certified sleep medicine specialists are experts in sleep disorders. We know how sleep affects a child’s body, behavior, learning and more.
11
8 hours
12+
Our Highlights
We have state-of-the-art sleep centers just for kids. We provide sleep studies in private, kid-friendly rooms. While your child sleeps, we can record a variety of body functions to help us understand what’s going on. You can sleep in the same room with your child, next to their bed.
We offer specialized sleep programs. Our teams work together to help kids with special health needs sleep better. We have expertise in neuromuscular disorders, epilepsy, autism spectrum disorders and craniofacial disorders.
We offer behavioral sleep therapies. Our sleep psychologists can help kids get to sleep, and stay asleep, using cognitive behavioral therapies and more. We work with kids who have nightmares, anxiety and other problems that affect good rest.
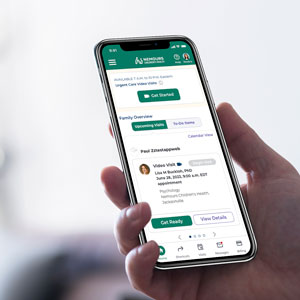
We Make It Easy With Online Video Visits
When several appointments are needed, we try to coordinate services so you only have to make one visit. And families can see a sleep specialist with our easy-to-use video-visit option. Whether it’s an introductory conversation, follow up visit, or a discussion about treatment, we can often save you travel time with our secure video connection.

Preparing for a Sleep Study
A sleep study (or polysomnogram) helps doctors diagnose sleep problems. It is an overnight test that can record body functions while a child sleeps. Learn what to expect during a sleep study.